Health Sector Transformation: A Unified E-Health Platform, AI-Driven Care, Digital Policy, Innovation, Industry 4.0/5.0 & Centralized Medical Process
Abstract
The convergence of artificial intelligence (AI), Industry 4.0 & 5.0 technologies, and digital transformation is reshaping healthcare worldwide. Industry 4.0 advanced automation through robotics, IoT, and cloud systems, while Industry 5.0 emphasizes human-centric innovation, ethical AI, and sustainability. Key applications include AI in diagnostics, drug discovery, health operations, robotics, and virtual care, supported by precision medicine, digital infrastructures, and intelligent operating rooms. Yet challenges in governance, financing, workforce readiness, and equity persist. Drawing on global frameworks such as the EU AI Act and WHO guidelines, this paper argues that inclusive governance and robust regulation are critical for equitable adoption. Guided by Industry 5.0 principles, countries can build resilient, sustainable, and patient-centered health systems that leave no population behind.
Introduction
Healthcare is entering a new era where AI, robotics, and digital platforms intersect with Industry 4.0 and 5.0. While Industry 4.0 prioritized automation and efficiency, Industry 5.0 shifts focus toward human-centric, ethical, and sustainable health innovation. This transformation is not only technological but also a governance and equity challenge of global importance.
Bangladesh is uniquely positioned within this transition. Its health system faces persistent pressures from rising non-communicable diseases, recurrent infectious outbreaks, high out-of-pocket spending, and fragmented health records. At the same time, rapid advances in AI, telemedicine, and digital health provide an opportunity to overcome workforce shortages and rural–urban disparities. The Health Sector Transformation Roadmap (2025–2035) and Bangladesh 2.0 vision prioritize digital health as a foundation for Universal Health Coverage (UHC). A Unified E-Health Platform (UEHP)—integrating centralized medical profiles, AI-assisted diagnostics, and predictive health intelligence—can serve as the backbone of this transformation. By ensuring interoperability, scalability, and equity, Bangladesh has the potential to emerge as a global model for digital-first, AI-enabled, and patient-centered health systems among low- and middle-income countries (LMICs).
Industry 4.0 to 5.0: Shifting Paradigms in Healthcare
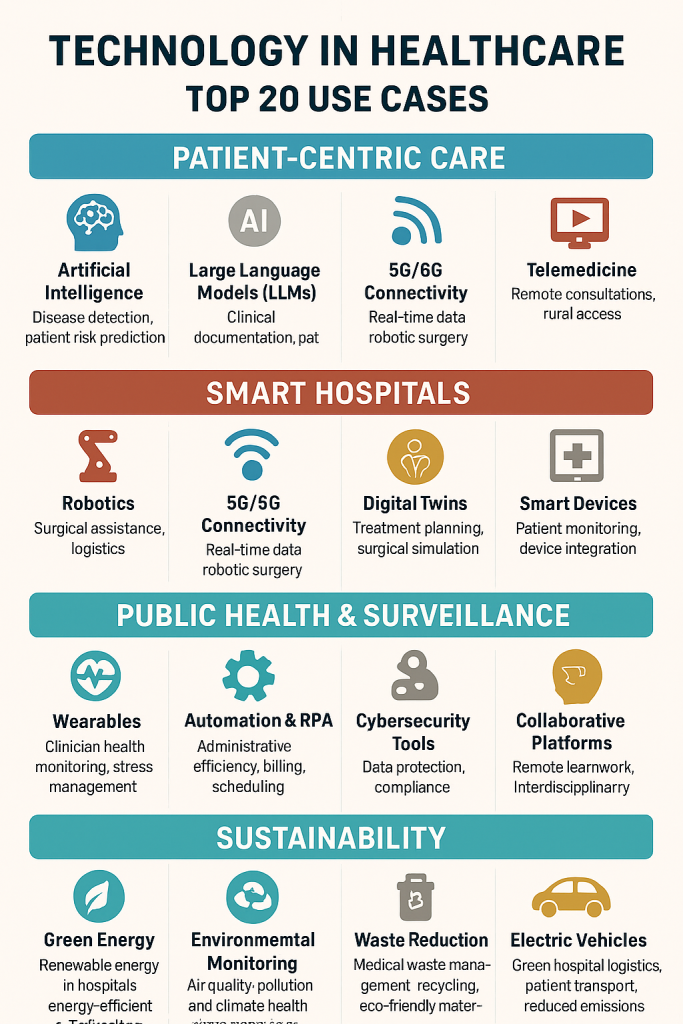
Industry 4.0 transformed healthcare through robotics, automation, the Internet of Things (IoT), and cloud computing, enabling smart hospitals, remote monitoring, and predictive maintenance of medical equipment. Industry 5.0 advances this trajectory by placing humans at the center of innovation. In healthcare, this means that AI and robotics are designed to complement clinicians, enhance decision-making, and improve patient experiences rather than prioritizing efficiency alone. The model emphasizes personalized medicine, patient empowerment, ethical AI, and sustainability.
Artificial Intelligence Across the Health Ecosystem
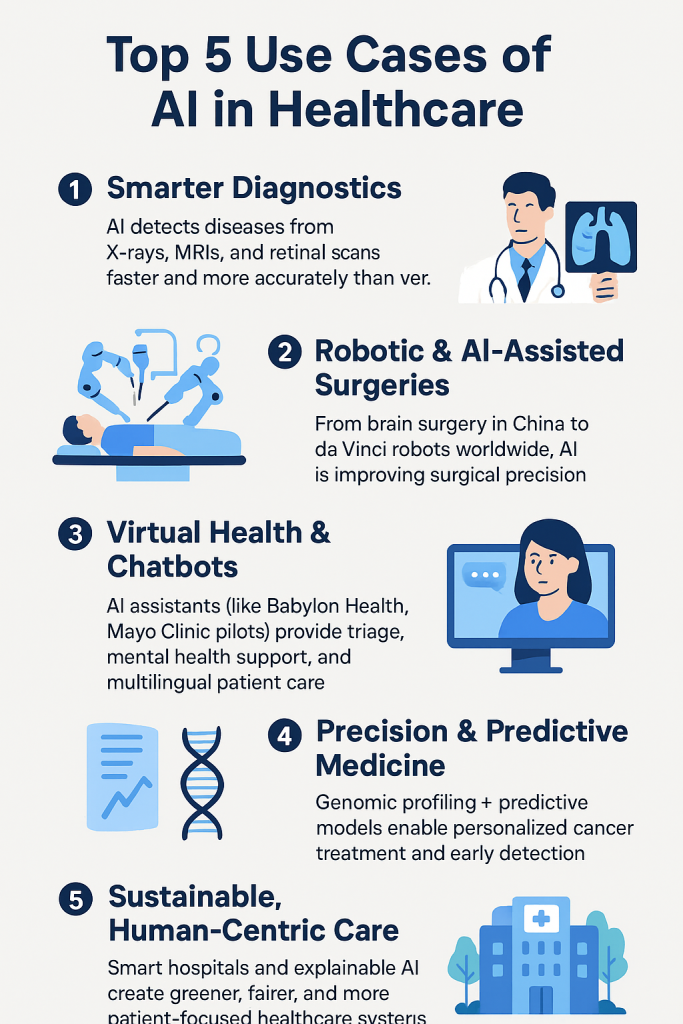
- Diagnostics & Imaging: Deep learning models now outperform human benchmarks in radiology and pathology. For example, Google DeepMind and Moorfields Eye Hospital (UK) developed an AI system capable of detecting more than 50 retinal diseases at par with expert ophthalmologists.
- Drug Discovery & Genomics: AI accelerates therapeutic discovery and enables individualized treatment based on genomic profiling. Foundation Medicine (USA) integrates genomic sequencing with AI to match cancer patients to targeted therapies.
- Operational Efficiency: AI-driven hospital management optimizes supply chains, predicts ICU demand, and supports workflow automation. Singapore’s health system has deployed AI forecasting tools to manage critical care resources during pandemics.
- Virtual Health & Telemedicine: Digital platforms supported by conversational AI and remote monitoring devices expand access to underserved populations, exemplified by Philips–WHO telehealth initiatives in Africa and Asia.
These applications have demonstrated measurable improvements, yet their integration into health systems raises policy concerns over standards, financing, and accountability.
Digital Transformation as a Backbone
Digital transformation integrates AI, big data analytics, 5G connectivity, and cybersecurity into unified health ecosystems. This enables:
- Integrated Health Records across borders and systems.
- Real-Time Public Health Data, as demonstrated by BlueDot (Canada), which flagged atypical pneumonia in Wuhan before WHO’s official alerts.
- Patient-Centered Platforms leveraging wearables, mobile apps, and personalized dashboards.
Realizing these opportunities requires alignment across ministries of health, finance, ICT regulators, and international agencies.
Robotics in Healthcare
Robotics is increasingly central to both clinical and operational domains.
- Surgical Robotics: The da Vinci Surgical System, used in more than 10 million procedures globally, has redefined minimally invasive surgery through enhanced dexterity and visualization.
- Rehabilitation Robotics: Ekso Bionics (USA) produces exoskeletons that allow stroke and spinal cord injury patients to regain mobility.
- Hospital Automation: Service robots manage disinfection, medication delivery, and logistics, freeing staff for patient-focused tasks.
Natural Language Processing (NLP) and Large Language Models (LLMs)
Healthcare generates massive volumes of unstructured data. NLP and LLMs provide actionable insights by:
- Automating clinical documentation (e.g., Mayo Clinic’s pilots of GPT-based assistants for electronic health record summarization).
- Enhancing evidence synthesis (IBM Watson Health pioneered oncology-focused cognitive computing).
- Improving patient communication (Babylon Health uses AI chatbots for triage and multilingual consultations).
Precision Medicine and Predictive Healthcare
AI and data-driven models are enabling personalized, anticipatory care.
- Precision Medicine: Japan’s National Cancer Center applies AI genomic analytics to personalize oncology treatment.
- Predictive Analytics: Hospitals in the Netherlands and Singapore forecast patient admissions and ICU occupancy to improve system resilience.
- Public Health Surveillance: BlueDot’s early COVID-19 detection illustrates the value of predictive models for epidemic preparedness.
AI-Assisted Surgeries and Intelligent Operating Rooms
Beyond robotics, AI supports surgical decision-making through:
- Preoperative planning using patient-specific imaging.
- Real-time intraoperative guidance.
- Training through augmented reality (AR) simulators, as explored in Microsoft–Johns Hopkins’ “intelligent operating rooms.”
Sustainable and Human-Centric Health Services
Industry 5.0 emphasizes sustainability and human-technology collaboration.
- Scandinavian smart hospitals use AI and IoT to reduce energy waste and medical inefficiency.
- WHO and Philips collaborate on AI-enabled telemedicine platforms to bridge rural healthcare gaps.
- EU-funded projects on explainable AI (XAI) seek to ensure transparency, fairness, and trust in clinical contexts.
Digital health and artificial intelligence (AI) offer a pathway to leapfrog traditional barriers by:
- Unifying patient data through Centralized Medical Profiles (CMPs).
- Establishing a Unified E-Health Platform (UEHP) for telemedicine, AI diagnostics, and real-time surveillance.
- Embedding predictive intelligence for population health planning and personalized care.
Technical Architecture of the Unified E-Health Platform
Core Components
- National Digital Health Stack (NDHS): Unique patient identifier linked to National ID (NID), HL7 FHIR-based interoperability standards, and APIs for private-sector integration.
- Electronic Health Records (EHR): Longitudinal records capturing patient history, prescriptions, lab tests, imaging, and vaccination.
- Telemedicine Module: Secure video/audio consultations with scheduling, digital prescriptions, and referral systems.
- AI Diagnostic Engine: Validated algorithms for radiology (TB, chest X-ray, ultrasound), dermatology (skin lesion detection), and cardiology (ECG interpretation).
- Analytics & Dashboards: Real-time disease surveillance, hospital capacity tracking, and predictive outbreak models.
Cybersecurity and Data Governance
- Zero-trust architecture with end-to-end encryption.
- National Health Data Policy defining data ownership, consent, and cross-border data transfer.
- AI assurance protocols aligned with WHO AI ethics and UNESCO AI principles.
Interoperability Framework
- Integration with existing health initiatives (DGHS MIS, DHIS2, eMIS for community clinics).
- Plug-and-play APIs for private telemedicine providers (e.g., Tonic, Praava, Maya).
- Cross-sector linkages with agriculture, environment, and disaster management for One Health integration.
Centralized Medical Profiles
Concept
A Centralized Medical Profile (CMP) is a longitudinal digital health record for every citizen, securely linked to the National ID (NID). It aggregates:
- Demographics, biometric data, and unique health identifiers.
- Medical history, diagnoses, prescriptions, lab results, and imaging.
- Immunization records, maternal/child health milestones, and chronic disease follow-ups.
- Patient-reported data from wearables, mobile apps, and remote monitoring.
Technical Architecture
- Data Layer: Cloud-based storage with redundancy and disaster recovery.
- Interoperability Layer: HL7 FHIR standards, ensuring seamless data exchange across hospitals, clinics, pharmacies, and labs.
- Access Layer: Role-based access (clinician, patient, policymaker) with strong authentication.
- Consent & Privacy: Patient-controlled sharing mechanisms, digital signatures, and blockchain audit trails.
Benefits
- Eliminates duplication of tests and prescriptions.
- Provides continuity of care across rural–urban divides.
- Enables population-level analytics for policy and planning.
Unified E-Health Platform
Concept
A Unified E-Health Platform (UEHP) is the backbone connecting CMPs with service delivery. Instead of fragmented apps or siloed systems, UEHP integrates all digital health services under a single interoperable ecosystem.
Core Modules
- Telemedicine: Video/audio consultations, digital prescriptions, eReferrals.
- AI Diagnostics: Radiology (X-rays, CT), dermatology (skin lesions), cardiology (ECG).
- Pharmacy Integration: E-prescriptions linked to drug supply chain and price transparency.
- Public Health Surveillance: Real-time dashboards for outbreaks, NCD trends, and facility readiness.
- One Health Linkages: Cross-sector data from veterinary, environmental, and climate systems.
Governance & Security
- National Health Digital & AI Council (H-DAC) for standards, procurement, and cybersecurity.
- Compliance with WHO Global Strategy on Digital Health.
- Public–private partnerships with telecoms for zero-rated telehealth access.
Predictive Intelligence & Personalized Recommendations
Concept
The power of CMP + UEHP lies in AI-driven analytics. Predictive models can use historical, clinical, and real-time data to anticipate risks, improve outcomes, and guide patient care.
Technical Features
- Machine Learning Models: Disease risk prediction (diabetes, hypertension, cardiovascular disease). Outbreak forecasting (dengue, diarrheal disease, TB). Resource optimization (hospital bed demand, oxygen supply, vaccine distribution).
- Recommendation Engines: Patient-facing: lifestyle guidance, medication reminders, preventive screenings. Provider-facing: clinical decision support, diagnostic suggestions, treatment optimization.
Policy-facing: predictive dashboards for planning and budget allocation. Current Challenges
- Fragmented Records: Lack of continuity of care across facilities.
- Limited Access: Rural and marginalized populations underserved.
- High Costs: >65% of health spending is out-of-pocket.
- System Strain: Climate-sensitive outbreaks (e.g., dengue) overstretch hospitals.
- Digital Divide: Unequal connectivity and literacy across regions.
Policy Framework
The proposed framework rests on three pillars:
Centralized Medical Profiles (CMPs)
- Longitudinal, citizen-linked health records tied to National ID.
- Integrated lab results, prescriptions, imaging, and maternal/child health milestones.
- Patient-controlled access and blockchain-enabled audit trails.
Unified E-Health Platform (UEHP)
- Backbone system integrating telemedicine, AI diagnostics, ePrescriptions, and public health surveillance.
- Interoperable via HL7 FHIR standards and governed by a Health Digital & AI Council (H-DAC).
- Pharmacy, lab, and insurance integration for seamless service delivery.
Predictive Intelligence & Recommendations
- Patient-facing: lifestyle reminders, preventive screenings, AI symptom triage.
- Provider-facing: decision support, diagnostic suggestions, clinical risk scores.
- Policy-facing: outbreak forecasting, resource allocation, NCD monitoring.
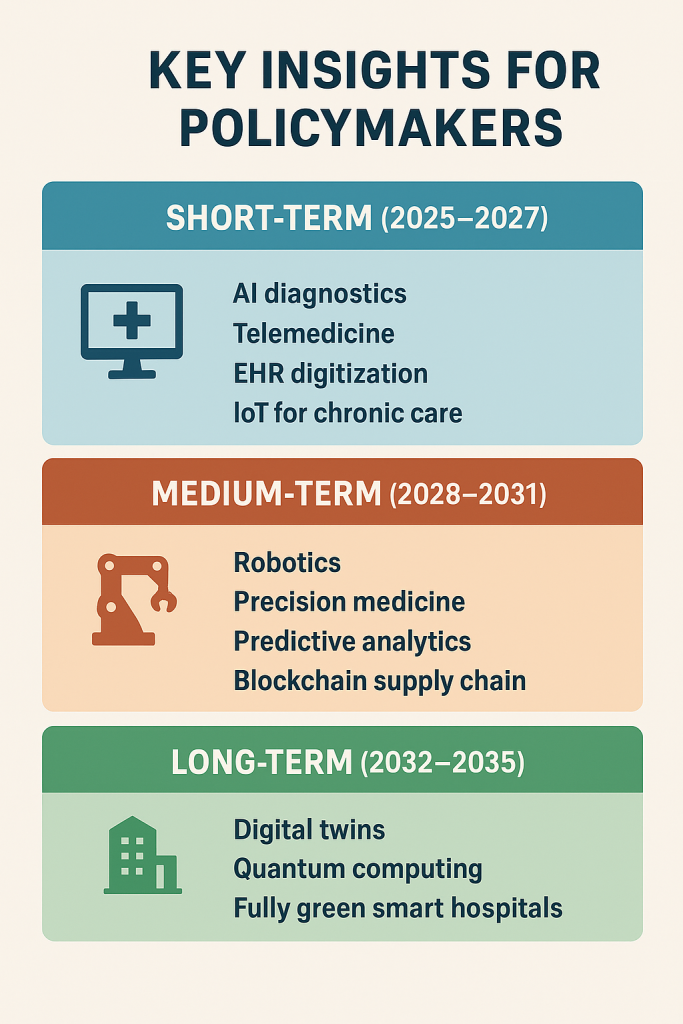
Implementation Roadmap (2025–2035)
Phase I – Foundations (2025–2027)
- Establish Health Digital & AI Council (H-DAC).
- Pilot CMPs in 3 digital districts.
- Launch interoperable telemedicine and AI-assisted TB/maternal health diagnostics.
Phase II – Expansion (2028–2031)
- Nationwide rollout of CMPs, telemedicine, and ePrescriptions.
- AI diagnostics for radiology, dermatology, and cardiology in district hospitals.
- Predictive analytics for NCDs and dengue outbreaks.
- Public spending increased to 2% of GDP, with ring-fenced digital health funding.
Phase III – Transformation (2032–2035)
- Universal CMP coverage with fully AI-augmented hospitals.
- Precision medicine pilots (genomics + AI).
- Climate-resilient “smart hospitals” powered by green energy and predictive operations.
- Regional health data exchanges (SAARC Digital Health Corridor).
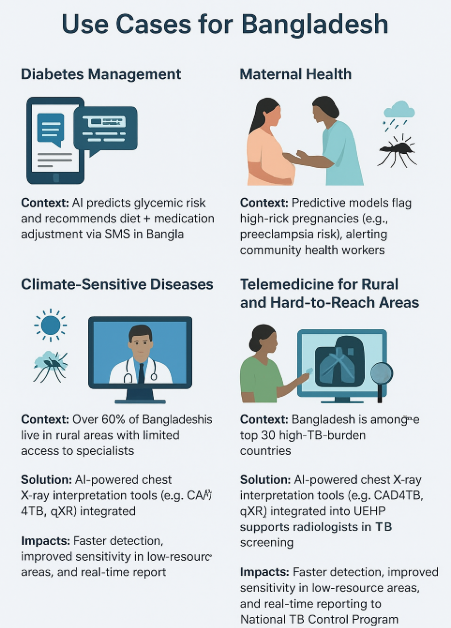
UseCases for Bangladesh
- Diabetes Management: AI predicts glycemic risk and recommends diet + medication adjustment via SMS in Bangla.
- Maternal Health: Predictive models flag high-risk pregnancies (e.g., preeclampsia risk), alerting community health workers.
- Climate-Sensitive Diseases: AI integrates weather data with health records to forecast dengue outbreaks, guiding targeted interventions.
Telemedicine for Rural and Hard-to-Reach Areas
- Context: Over 60% of Bangladeshis live in rural areas with limited access to specialists.
- Solution: The UEHP can deploy district-level telemedicine hubs connected to tertiary hospitals. Frontline health assistants can facilitate video consultations, supported by AI-based triage tools to prioritize urgent cases.
- Impact: Reduced referral overload at urban hospitals, lower travel costs, and faster diagnosis.
AI-Assisted Radiology in TB and Lung Health
- Context: Bangladesh is among the top 30 high-TB-burden countries.
- Solution: AI-powered chest X-ray interpretation tools (e.g., CAD4TB, qXR) integrated into the UEHP can support radiologists in TB screening.
- Impact: Faster detection, improved sensitivity in low-resource areas, and real-time reporting to the National TB Control Program.
Maternal & Child Health Monitoring
- Context: Maternal mortality (173/100,000 live births) remains a concern, particularly in rural regions.
- Solution: Tele-obstetrics with AI-enabled ultrasound interpretation, combined with remote monitoring (blood pressure, glucose sensors). Alerts can be escalated to specialists in urban centers.
- Impact: Early identification of preeclampsia, gestational diabetes, and complications—reducing maternal and neonatal mortality.
NCD Management via Digital Pathways
- Context: NCDs (cardiovascular disease, diabetes) account for >67% of deaths.
- Solution: AI-powered risk calculators embedded in EHR, with teleconsultations for routine follow-up. E-prescriptions linked to pharmacy supply chains and SMS medication reminders.
- Impact: Improved adherence, reduced catastrophic spending, and early interventions.
Emergency Response & Climate Resilience
- Context: Floods, cyclones, and heatwaves disrupt healthcare delivery.
- Solution: UEHP dashboards can integrate satellite/weather data with health facility information to anticipate service disruptions. AI models can predict dengue or diarrheal outbreaks based on climate trends.
- Impact: Stronger health system resilience in the face of climate change.
Toward Human-Centric and Sustainable Health Systems
Industry 5.0 emphasizes the co-evolution of technology and human expertise, aligning with principles of sustainability, inclusivity, and patient-centeredness. Key pathways include:
- Sustainable Digital Health: Smart hospitals with reduced environmental footprints.
- Equitable Access: Digital health platforms targeted at rural and underserved populations.
- Trust and Accountability: Promoting explainable AI to build clinician and patient confidence.
- International Collaboration: Cross-border data-sharing frameworks for global disease surveillance and precision medicine.
Regulatory Frameworks
Global regulatory frameworks are evolving to strengthen safety, transparency, and equity. Policymakers across jurisdictions are now prioritizing these issues as part of broader governance and compliance agendas.:
- European Union (EU AI Act): Classifies healthcare AI as “high risk,” requiring human oversight, transparency, and strict data governance.
- United States (FDA Digital Health Program): Approves AI-driven diagnostic tools while piloting frameworks for adaptive algorithms.
- World Health Organization (WHO): Provides global guidance on equity, transparency, and human rights in AI adoption.
- Asia (China, Japan): Combining major investment in precision medicine AI and robotic surgery with tightening regulations on data privacy.
These examples reflect a growing consensus that AI in health requires proactive regulation, not retrospective correction.
Challenges and Ethical Considerations
Despite rapid advances, digital transformation in healthcare presents systemic challenges:
- Data Privacy and Security: Protection of sensitive health data in increasingly interconnected systems.
- Algorithmic Transparency: Ensuring AI tools are explainable, unbiased, and ethically governed.
- Digital Divide: Mitigating inequalities between high- and low-income countries in access to infrastructure, skills, and financing.
- Health Workforce Adaptation: Preparing professionals to collaborate with AI systems while safeguarding professional autonomy.
- Ethical AI, requires transparency, bias mitigation, and explainability.
These challenges highlight the need for global governance frameworks that balance innovation with equity and ethics.
Policy Implications
- Governance: Strong stewardship by MoHFW, ICT, and Finance ministries to align digital standards, procurement, and regulation.
- Equity: Zero-rated data packages for telehealth, inclusive design for Rohingya and marginalized populations, and gender-responsive services.
- Financing: Public–private partnerships and innovative financing for digital infrastructure.
- Capacity: Digital literacy programs and integration of AI into medical/nursing curricula.
- Ethics & Privacy: National Health Data Policy ensuring transparency, consent, and AI bias mitigation.
Conclusion: The Road Ahead
The convergence of AI, Industry 4.0/5.0, and digital transformation is reshaping global healthcare, offering advances in precision medicine, predictive public health, and sustainable systems. However, realizing these benefits depends on inclusive governance, ethical regulation, and equitable adoption.
Bangladesh’s Health Sector Transformation Roadmap (2025–2035) embodies this vision by integrating governance reform, digital health infrastructure, ethical AI, and equity-focused delivery. Anchored in Centralized Medical Profiles, a Unified E-Health Platform, and Predictive Health Intelligence, the roadmap positions Bangladesh to leapfrog systemic barriers and build a resilient, patient-centered, and climate-ready health system. If implemented effectively, it could serve as a global model for LMICs advancing Universal Health Coverage (UHC) through digital innovation.
Engr. Johnny Shahinur Alam
Technologist and ICT & Digital Transformation Specialist


